Description:
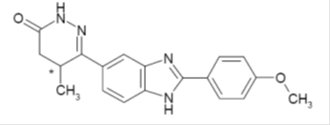
Vetmedin (pimobendan) is supplied as oblong half-scored chewable tablets containing 1.25, 2.5, 5 or 10 mg pimobendan per tablet. Pimobendan, a benzimidazole-pyridazinone derivative, is a non-sympathomimetic, non-glycoside inotropic drug with vasodilatative properties. Pimobendan exerts a stimulatory myocardial effect by a dual mechanism of action consisting of an increase in calcium sensitivity of cardiac myofilaments and inhibition of phosphodiesterase (Type III). Pimobendan exhibits vasodilating activity by inhibiting phosphodiesterase III activity. The chemical name of pimobendan is 4,5-dihydro-6-[2-(4-methoxyphenyl)-1H-benzimidazole-5-yl]-5-methyl-3(2H)-pyridazinone. The structural formula of pimobendan is:
Indications:
Vetmedin (pimobendan) is indicated for the management of the signs of mild, moderate, or severe (modified NYHA Class IIa, IIIb, or IVc) congestive heart failure in dogs due to atrioventricular valvular insufficiency (AVVI) or dilated cardiomyopathy (DCM). Vetmedin is indicated for use with concurrent therapy for congestive heart failure (e.g., furosemide, etc.) as appropriate on a case-by-case basis.
a A dog with modified New York Heart Association (NYHA) Class II heart failure has fatigue, shortness of breath, coughing, etc. apparent when ordinary exercise is exceeded.
b A dog with modified NYHA Class III heart failure is comfortable at rest, but exercise capacity is minimal.
c A dog with modified NYHA Class IV heart failure has no capacity for exercise and disabling clinical signs are present even at rest.
Dosage and Administration:
Vetmedin should be administered orally at a total daily dose of 0.23 mg/lb (0.5 mg/kg) body weight, using a suitable combination of whole or half tablets. The total daily dose should be divided into 2 portions that are not necessarily equal, and the portions should be administered approximately 12 hours apart (i.e., morning and evening). The tablets are scored and the calculated dosage should be provided to the nearest half tablet increment.
Contraindications:
Vetmedin should not be given in cases of hypertrophic cardiomyopathy, aortic stenosis, or any other clinical condition where an augmentation of cardiac output is inappropriate for functional or anatomical reasons.
Warnings:
Only for use in dogs with clinical evidence of heart failure. At 3 and 5 times the recommended dosage, administered over a 6-month period of time, pimobendan caused an exaggerated hemodynamic response in the normal dog heart, which was associated with cardiac pathology (See Animal Safety).
Human Warnings:
Not for use in humans. Keep this and all medications out of reach of children. Consult a physician in case of accidental ingestion by humans.
Precautions:
The safety of Vetmedin has not been established in dogs with asymptomatic heart disease or in heart failure caused by etiologies other than AVVI or DCM. The safe use of Vetmedin has not been evaluated in dogs younger than 6 months of age, dogs with congenital heart defects, dogs with diabetes mellitus or other serious metabolic diseases, dogs used for breeding, or pregnant or lactating bitches.
Adverse Reactions:
Clinical findings/adverse reactions were recorded in a 56-day field study of dogs with congestive heart failure (CHF) due to AVVI (256 dogs) or DCM (99 dogs). Dogs were treated with either Vetmedin (175 dogs) or the active control enalapril maleate (180 dogs). Dogs in both treatment groups received additional background cardiac therapy (See Effectiveness for details and the difference in digoxin administration between treatment groups).
The Vetmedin group had the following prevalence (percent of dogs with at least one occurrence) of common adverse reactions/new clinical findings (not present in a dog prior to beginning study treatments): poor appetite (38%), lethargy (33%), diarrhea (30%), dyspnea (29%), azotemia (14%), weakness and ataxia (13%), pleural effusion (10%), syncope (9%), cough (7%), sudden death (6%), ascites (6%), and heart murmur (3%). Prevalence was similar in the active control group. The prevalence of renal failure was higher in the active control group (4%) compared to the Vetmedin group (1%).
Adverse reactions/new clinical findings were seen in both treatment groups and were potentially related to CHF, the therapy of CHF, or both. The following adverse reactions/new clinical findings are listed according to body system and are not in order of prevalence: CHF death, sudden death, chordae tendineae rupture, left atrial tear, arrhythmias overall, tachycardia, syncope, weak pulses, irregular pulses, increased pulmonary edema, dyspnea, increased respiratory rate, coughing, gagging, pleural effusion, ascites, hepatic congestion, decreased appetite, vomiting, diarrhea, melena, weight loss, lethargy, depression, weakness, collapse, shaking, trembling, ataxia, seizures, restlessness, agitation, pruritus, increased water consumption, increased urination, urinary accidents, azotemia, dehydration, abnormal serum electrolyte, protein, and glucose values, mild increases in serum hepatic enzyme levels, and mildly decreased platelet counts.
See Table 1 for mortality due to CHF (including euthanasia, natural death, and sudden death) and for the development of new arrhythmias (not present in a dog prior to beginning study treatments) by treatment group and type of heart disease (AVVI or DCM) in the 56-day field study.
Vetmedin Group |
Active Control Group |
|
Dogs that died due to CHF |
14.3% n = 175 9 of 126 dogs with AVVI 16 of 49 dogs with DCM |
14.4% n = 180 16 of 130 dogs with AVVI 10 of 50 dogs with DCM |
Dogs that developed new arrhythmiasa |
39.4% n = 175 45 of 126 dogs with AVVI 24 of 49 dogs with DCM |
45.0% n = 180 59 of 130 dogs with AVVI 22 of 50 dogs with DCM |
a New arrhythmias included supraventricular premature beats and tachycardia, atrial fibrillation, atrioventricular block, sinus bradycardia, ventricular premature beats and tachycardia, and bundle branch block.
Following the 56-day masked field study, 137 dogs in the Vetmedin group were allowed to continue on Vetmedin in an open-label extended-use study without restrictions on concurrent therapy. The adverse reactions/new clinical findings in the extended-use study were consistent with those reported in the 56-day study, with the following exception: One dog in the extended-use study developed acute cholestatic liver failure after 140 days on Vetmedin and furosemide.
In foreign post-approval drug experience reporting, the following additional suspected adverse reactions were reported in dogs treated with a capsule formulation of pimobendan: hemorrhage, petechia, anemia, hyperactivity, excited behavior, erythema, rash, drooling, constipation, and diabetes mellitus.
To report suspected adverse reactions, to obtain a Material Safety Data Sheet, or for technical assistance call 1-866-638-2226.
Clinical Pharmacology:
Pimobendan is oxidatively demethylated to a pharmacologically active metabolite which is then conjugated with sulfate or glucuronic acid and excreted mainly via feces. The mean extent of protein binding of pimobendan and the active metabolite in dog plasma is >90%. Following a single oral administration of 0.25 mg/kg Vetmedin tablets the maximal mean (± 1 SD) plasma concentrations (Cmax) of pimobendan and the active metabolite were 3.09 (0.76) ng/ml and 3.66 (1.21) ng/ml, respectively. Individual dog Cmax values for pimobendan and the active metabolite were observed 1 to 4 hours post-dose (mean: 2 and 3 hours, respectively). The total body clearance of pimobendan was approximately 90 mL/min/kg, and the terminal elimination half-lives of pimobendan and the active metabolite were approximately 0.5 hours and 2 hours, respectively. Plasma levels of pimobendan and active metabolite were below quantifiable levels by 4 and 8 hours after oral administration, respectively. The steady-state volume of distribution of pimobendan is 2.6 L/kg indicating that the drug is readily distributed into tissues. Food decreased the bioavailability of an aqueous solution of pimobendan, but the effect of food on the absorption of pimobendan from Vetmedin tablets is unknown.
In normal dogs instrumented with left ventricular (LV) pressure transducers, pimobendan increased LV dP/dtmax (a measure of contractility of the heart) in a dose dependent manner between 0.1 and 0.5 mg/kg orally. The effect was still present 8 hours after dosing. There was a delay between peak blood levels of pimobendan and active metabolite and the maximum physiologic response (peak LV dP/dtmax). Blood levels of pimobendan and active metabolite began to drop before maximum contractility was seen. Repeated oral administration of pimobendan did not result in evidence of tachyphylaxis (decreased positive inotropic effect) or drug accumulation (increased positive inotropic effect). Laboratory studies indicate that the positive inotropic effect of pimobendan may be attenuated by the concurrent use of a β-adrenergic blocker or a calcium channel blocker.
Effectiveness:
In a double-masked, multi-site, 56-day field study, 355 dogs with modified NYHA Class II, III, or IV CHF due to AVVI or DCM were randomly assigned to either the active control (enalapril maleate) or the Vetmedin (pimobendan) treatment group. Of the 355 dogs, 52% were male and 48% were female; 72% were diagnosed with AVVI and 28% were diagnosed with DCM; 34% had Class II, 47% had Class III, and 19% had Class IV CHF. Dogs ranged in age and weight from 1 to 17 years and 3.3 to 191 lb, respectively. The most common breeds were mixed breed, Doberman Pinscher, Cocker Spaniel, Miniature/Toy Poodle, Maltese, Chihuahua, Miniature Schnauzer, Dachshund, and Cavalier King Charles Spaniel. The 180 dogs (130 AVVI, 50 DCM) in the active control group received enalapril maleate (0.5 mg/kg once or twice daily), and all but 2 received furosemide. Per protocol, all dogs with DCM in the active control group received digoxin. The 175 dogs (126 AVVI, 49 DCM) in the Vetmedin group received pimobendan (0.5 mg/kg/day divided into 2 portions that were not necessarily equal, and the portions were administered approximately 12 hours apart), and all but 4 received furosemide. Digoxin was optional for treating supraventricular tachyarrhythmia in either treatment group, as was the addition of a β-adrenergic blocker if digoxin was ineffective in controlling heart rate. After initial treatment at the clinic on Day 1, dog owners were to administer the assigned product and concurrent medications for up to 56±4 days.
The determination of effectiveness (treatment success) for each case was based on improvement in at least 2 of the 3 following primary variables: modified NYHA classification, pulmonary edema score by a masked veterinary radiologist, and the investigator’s overall clinical effectiveness score (based on physical examination, radiography, electrocardiography, and clinical pathology). Attitude, pleural effusion, coughing, activity level, furosemide dosage change, cardiac size, body weight, survival, and owner observations were secondary evaluations contributing information supportive to product effectiveness and safety.
Based on protocol compliance and individual case integrity, 265 cases (134 Vetmedin, 131 active control) were evaluated for treatment success on Day 29. See Table 2 for effectiveness results.
Vetmedin Group |
Active Control Group |
|
Treatment Success on Day 29 |
80.7% n = 134 88 of 101 dogs with AVVI 20 of 33 dogs with DCM |
76.3% n = 131 77 of 100 dogs with AVVI 23 of 31 dogs with DCM |
Treatment Success on Day 56 |
71.1% n = 113 66 of 85 dogs with AVVI 13 of 28 dogs with DCM |
67.2% n = 110 56 of 85 dogs with AVVI 17 of 25 dogs with DCM |
No increase in furosemide dose between Day 1 and Day 29 |
78.3% n = 130 |
68.6% n = 126 |
At the end of the 56-day study, dogs in the Vetmedin group were enrolled in an unmasked field study to monitor safety under extended use, without restrictions on concurrent medications.
Vetmedin was used safely in dogs concurrently receiving furosemide, digoxin, enalapril, atenolol, spironolactone, nitroglycerin, hydralazine, diltiazem, antiparasitic products (including heartworm prevention), antibiotics (metronidazole, cephalexin, amoxicillin-clavulanate, fluoroquinolones), topical ophthalmic and otic products, famotidine, theophylline, levothyroxine sodium, diphenhydramine, hydrocodone, metoclopramide, and butorphanol, and in dogs on sodium-restricted diets.
Palatability:
In a laboratory study, the palatability of Vetmedin was evaluated in 20 adult female Beagle dogs offered doses twice daily for 14 days. Ninety percent (18 of 20 dogs) voluntarily consumed more than 70% of the 28 tablets offered. Including two dogs that consumed only 4 and 7% of the tablets offered, the average voluntary consumption was 84.2%.
Animal Safety:
In a laboratory study, Vetmedin chewable tablets were administered to 6 healthy Beagles per treatment group at 0 (control), 1, 3, and 5 times the recommended dosage for 6 months. See Table 3 for cardiac pathology results. The cardiac pathology/histopathology noted in the 3X and 5X dose groups is typical of positive inotropic and vasodilator drug toxicity in normal dog hearts, and is associated with exaggerated hemodynamic responses to these drugs. None of the dogs developed signs of heart failure and there was no mortality.
Severe left ventricular hypertrophy with multifocal subendocardial ischemic lesions |
One 3X and two 5X dogsa |
Moderate to marked myxomatous thickening of the mitral valves |
Three 5X dogs |
Myxomatous thickening of the chordae tendineae |
One 3X and two 5X dogs |
Endocardial thickening of the left ventricular outflow tract |
One 1X, two 3X, and two 5X dogs |
Left atrial endocardial thickening (jet lesions) in 2 of the dogs that developed murmurs of mitral valve insufficiency |
One 3X and one 5X dog |
Granulomatous inflammatory lesion in the right atrial myocardium |
One 3X dog |
a Most of the gross and histopathologic findings occurred in these three dogs
Murmurs of mitral valve insufficiency were detected in one 3X (Day 65) and two 5X dogs (Days 135 and 163). These murmurs (grades II-III of VI) were not associated with clinical signs.
Indirect blood pressure was unaffected by Vetmedin at the label dose (1X). Mean diastolic blood pressure was decreased in the 3X group (74 mmHg) compared to the control group (82 mmHg). Mean systolic blood pressure was decreased in the 5X group (117 mmHg) compared to the control group (124 mmHg). None of the dogs had clinical signs of hypotension.
On 24-hour Holter monitoring, mean heart rate was increased in the 5X group (101 beats/min) compared to the control group (94 beats/min). Not counting escape beats, the 3X and 5X groups had slightly higher numbers of isolated ventricular ectopic complexes (VEs). The maximum number of non-escape VEs recorded either at baseline or in a control group dog was 4 VEs/24 hours. At either Week 4 or Week 20, three 3X group dogs had maximums of 33, 13, and 10 VEs/24 hours, and two 5X group dogs had maximums of 22 and 9 VEs/24 hours. One 1X group dog with no VEs at baseline had 6 VEs/24 hours at Week 4 and again at Week 20. Second-degree atrioventricular heart block was recorded in one 3X group dog at Weeks 4 and 20, and in one dog from each of the 1X and 5X groups at Week 20. None of the dogs had clinical signs associated with these electrocardiogram changes.
Treatment was associated with small differences in mean platelet counts (decreased in the 3X and 1X groups), potassium (increased in the 5X group), glucose (decreased in the 1X and 3X groups), and maximum blood glucose in glucose curves (increased in the 5X group). All individual values for these variables were within the normal range. Three 1X and one 5X group dogs had mild elevations of alkaline phosphatase (less than two times normal).
Loose stools and vomiting were infrequent and self-limiting.
Storage Information:
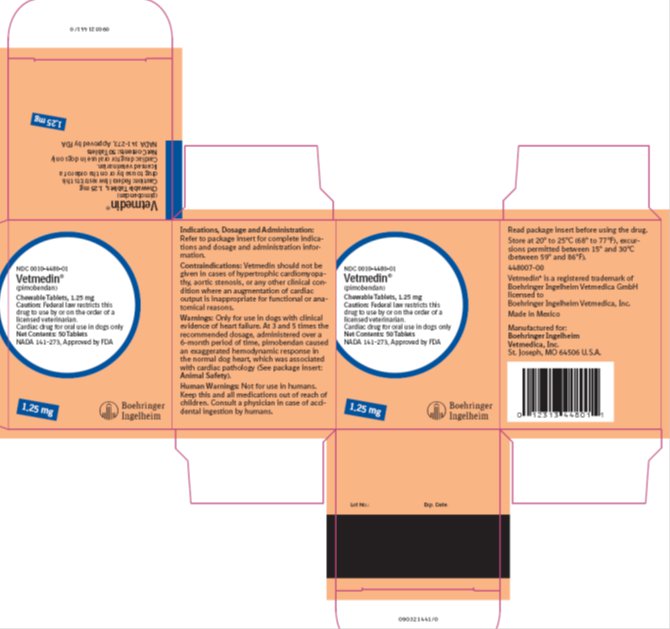
Store at 20° to 25°C (68° to 77°F), excursions permitted between 15° and 30°C (between 59° and 86°F).
How Supplied:
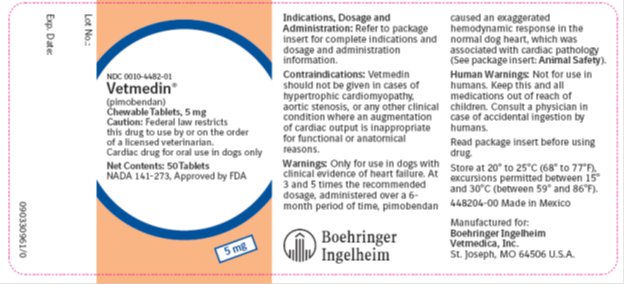
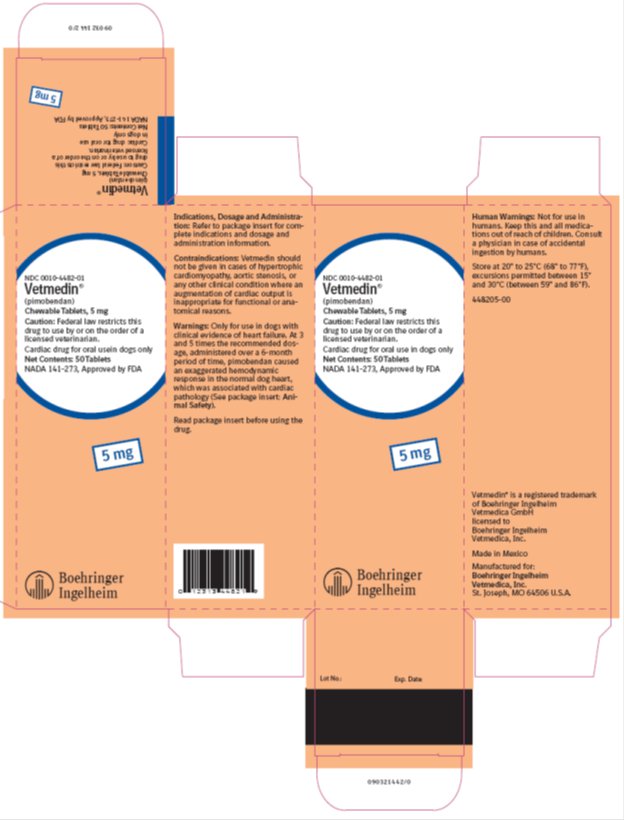
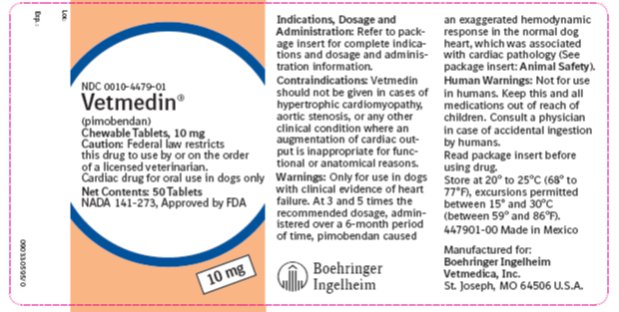
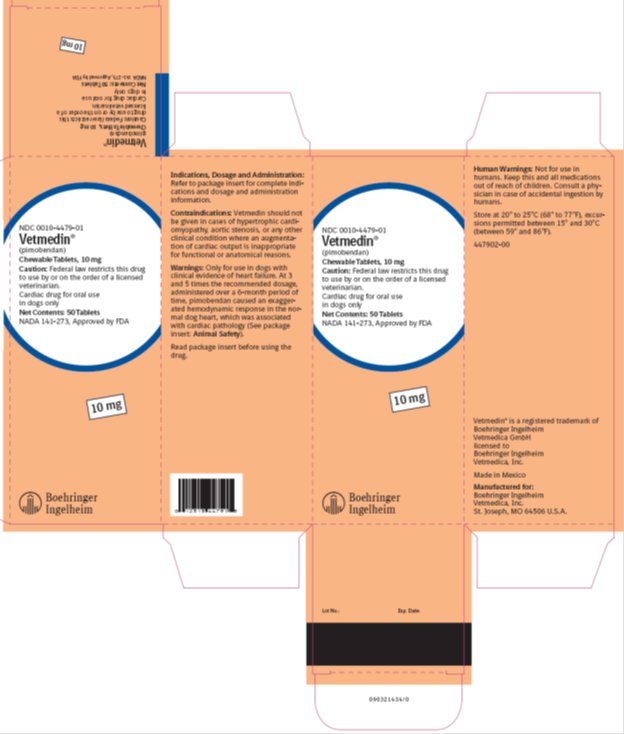
Vetmedin (pimobendan) Chewable Tablets:
Available as 1.25, 2.5, 5 and 10 mg oblong half-scored chewable tablets – 50 tablets per bottle.
NDC 0010-4480-01 - 1.25 mg - 50 tablets
NDC 0010-4481-01 – 2.5 mg – 50 tablets
NDC 0010-4482-01 - 5 mg - 50 tablets
NDC 0010-4479-01 – 10 mg – 50 tablets
Vetmedin is a registered trademark of Boehringer Ingelheim Vetmedica GmbH, licensed to Boehringer Ingelheim Vetmedica, Inc.
Copyright © 2013 Boehringer Ingelheim Vetmedica, Inc. or an affiliated company. All Rights Reserved.
Manufactured for:
Boehringer Ingelheim Vetmedica, Inc.
St. Joseph, MO 64506 U.S.A.
448005-00
Revised 06/2013